Correlation between Body Mass Index and Waist-Hip Ratio amongst First Year Medical Students in Central Gujarat, India
2Associate Professor, Department of Community Medicine, Government Medical College Baroda, India
3Assistant Professor, Department of Community Medicine, Government Medical College Baroda, India
Abstract
Introduction:Body Mass Index (BMI) and Waist–Hip Ratio (WHR) are common anthropometric indices to assess adiposity. However, BMI does not distinguish between lean mass and fat distribution, which limit its accuracy in identifying central obesity. This study aimed to assess the correlation between BMI and WHR among first-year medical students and to compare obesity prevalence based on these indices. Methods: A cross-sectional study was conducted among first-year medical students. Anthropometric measurements, including height, weight, waist and hip circumference, were recorded using standardised methods. WHO criteria used for BMI, WHR was interpreted using gender-specific cut-offs for central obesity. The correlation between BMI and WHR was evaluated using Pearson’s correlation coefficient, and agreement between the two classifications was assessed using the Kappa statistic. Results: Most participants had BMI and WHR values within normal limits. The overall prevalence of overweight and obesity based on BMI was modest, higher among males than females. However, when assessed using WHR, central obesity was found to be more prevalent among males. No significant correlation was observed between BMI and WHR (r≈0). The Kappa statistic (κ=0.019; SE=0.076; 95%CI) indicated only slight agreement between BMI- and WHR-based classifications, suggesting that these indices measure different aspects of body composition. Conclusion: BMI and WHR reflect distinct dimensions of adiposity. Relying solely on BMI may underestimate central obesity, particularly in males. Routine use of both BMI and WHR in health screening among young adults is recommended for early identification of individuals at risk for non-communicable diseases.
Keywords: Adiposity, Adolescent, Body Mass Index, Waist-Hip Ratio
Introduction
Obesity has emerged as a global epidemic, rapidly transforming disease profiles across the world, particularly within low and middle-income countries. Defined as a disease characterized by excessive body fat, obesity is a serious public health concern, contributing to approximately 2.8 million deaths globally every year.[1] It serves as an independent risk factor for cardiovascular disease (CVD) and is linked to numerous serious medical conditions, including diabetes, hypertension, and stroke, leading to increased morbidity, mortality, and reduced life expectancy. The rising prevalence of overweight and obese youth is especially concerning, as childhood obesity is associated with an increased risk of adult obesity and various cardiovascular disease risk factors.[2]
In assessing body composition, Body Mass Index (BMI) calculated as weight in kilograms divided by height in meters squared is the widely utilized medical definition and screening tool for overall obesity.[3] However, the distribution of fat is crucial, making the assessment of central obesity critical for predicting health risks. The Waist Hip Ratio (WHR) is a specific indicator used to measure central adiposity, which research suggests is a better predictor of obesity-related complications like metabolic syndrome and the future chances of developing CVD. People with "apple-shaped" bodies (more weight around the waist) are known to face greater health risks compared to those with "pear-shaped" bodies (more weight carried around the hips).
Therefore, a primary objective of relevant studies is to determine the status and prevalence of obesity among youth using BMI, to assess the presence and prevalence of central obesity using WHR, and critically, to analyse the correlation between BMI and WHR. Understanding this relationship helps evaluate the efficiency of these anthropometric measures as screening tools for detecting overweight and obesity in the population. While some studies demonstrate a statistically significant correlation between BMI and WHR, particularly among female subjects, others have found no significant correlation among overall or male participants, emphasizing the need for continued investigation.
Methods
Study Design: A cross-sectional study was conducted to determine the correlation between Body Mass Index (BMI) and Waist-Hip Ratio (WHR) among first-year medical students.
Study Setting and Population: The study was carried out at one of the Medical College in Central Gujarat. The study population comprised MBBS students enrolled at the college during their first academic year.
Sample Size and Sampling Technique: A total of 234 students who provided informed consent were included in the study. Participants were selected using universal sampling, as all eligible and consenting first-year students were enrolled in the study.
Inclusion and Exclusion Criteria: All first-year MBBS students who provided written informed consent and were available at the time of data collection were included and students with any chronic illness or physical deformity that could influence anthropometric measurements were excluded.
Data Collection and Measurements: Each participant underwent anthropometric assessment following standard procedures by the Principal Investigator. Height (in cm) was measured using a stadiometer with participants standing barefoot. Weight (in kg) was recorded using a calibrated digital weighing scale with participants in light clothing and without shoes. Waist Circumference (WC) was measured at the midpoint between the lower margin of the last palpable rib and the top of the iliac crest using a non-elastic measuring tape. Hip Circumference (HC) was measured at the level of the greatest protrusion of the buttocks.
Body Mass Index (BMI) was calculated using the formula: BMI = Weight (kg)/ [Height (m)]². Classification was done according to Asian BMI criteria (Underweight: <18.5 kg/m², Normal: 18.5–22.9 kg/m², Overweight: 23.0–24.9 kg/m², Obese: ≥25.0 kg/m²).[4] Waist-Hip Ratio (WHR) was calculated using: WHR = Waist Circumference (cm)/ Hip Circumference (cm). Classification was done based on WHO standards (For males: Normal <0.90, Obese ≥0.90; For females: Normal <0.85, Obese ≥0.85).[5]
Data Analysis: Data was entered into Microsoft Excel and analysed using statistical software Epi info. Descriptive statistics were calculated for all variables. The correlation between BMI and WHR was assessed using Pearson’s correlation coefficient (r). A p-value of <.05 was considered statistically significant. The agreement between BMI and WHR was calculated through Kappa Statistics.
The level of agreement between BMI-based and WHR-based classifications was evaluated using Cohen’s Kappa (κ) statistic.[6] The strength of agreement was interpreted as follows: κ < 0 indicated no agreement; κ = 0.00–0.20 indicated slight agreement; κ = 0.21–0.40 indicated fair agreement; κ = 0.41–0.60 indicated moderate agreement; κ = 0.61–0.80 indicated substantial agreement; and κ = 0.81–1.00 indicated almost perfect agreement. These thresholds were used to assess the concordance between BMI and WHR classifications.
Ethical Considerations: The study protocol was approved by the Institutional Ethics Committee of Medical College Baroda. Written informed consent was obtained from all participants prior to inclusion in the study. Confidentiality of participant information was maintained throughout the research process.
Results
A total of 234 first-year MBBS students participated in the study. Among them, 169 (72%) were males and 65 (28%) were females. The median age of the participants was 18 (IQR-19 to 21) years.
| Variable | Males (n = 169) | Females (n = 65) |
|---|---|---|
| BMI Category | ||
| Underweight | 25 (14.8%) | 15 (23.1%) |
| Normal | 110 (65.1%) | 40 (61.5%) |
| Overweight | 22 (13.0%) | 8 (12.3%) |
| Obese | 12 (7.1%) | 2 (3.1%) |
| WHR Category | ||
| Normal | 115 (68.0%) | 52 (80.0%) |
| Central Obesity | 54 (32.0%) | 13 (20.0%) |
Based on the Asian BMI criteria, nearly 20% of male students and 15% of female students were categorised as overweight and Obese. The proportion of overweight and obese students was higher among males compared to females. According to WHO standards for WHR, 32% of males had WHR ≥0.90 indicating central obesity, while 20% females had WHR ≥0.85. This pattern suggests that central adiposity was more common among males even when BMI values were within normal limits. This suggest that central obesity is more observed as compared to overall body weight. (Table 1)
The level of agreement between BMI-based and WHR-based classifications of obesity was assessed using Cohen’s Kappa (κ) statistic. (Table 2) The observed agreement between the two measures was 99 (56.9%), while the agreement expected by chance was 97.6 (56.1%). The calculated Kappa value was 0.019 (SE = 0.076; 95% CI: -0.130, 0.168), indicating slight, but non-significant agreement between the two classification methods according to standard interpretation criteria.
| Waist–Hip Ratio | BMI* | Total | |
|---|---|---|---|
| Normal | Overweight | ||
| Normal | 80 | 41 | 121 |
| Overweight | 34 | 19 | 51 |
| Total | 114 | 60 | 174 |
Note. *Underweight students as per BMI were excluded for this calculation.
The correlation analysis between BMI and WHR revealed no significant linear relationship (p >.05). The strength of linear association between variables was assessed using Pearson’s correlation coefficient (r).
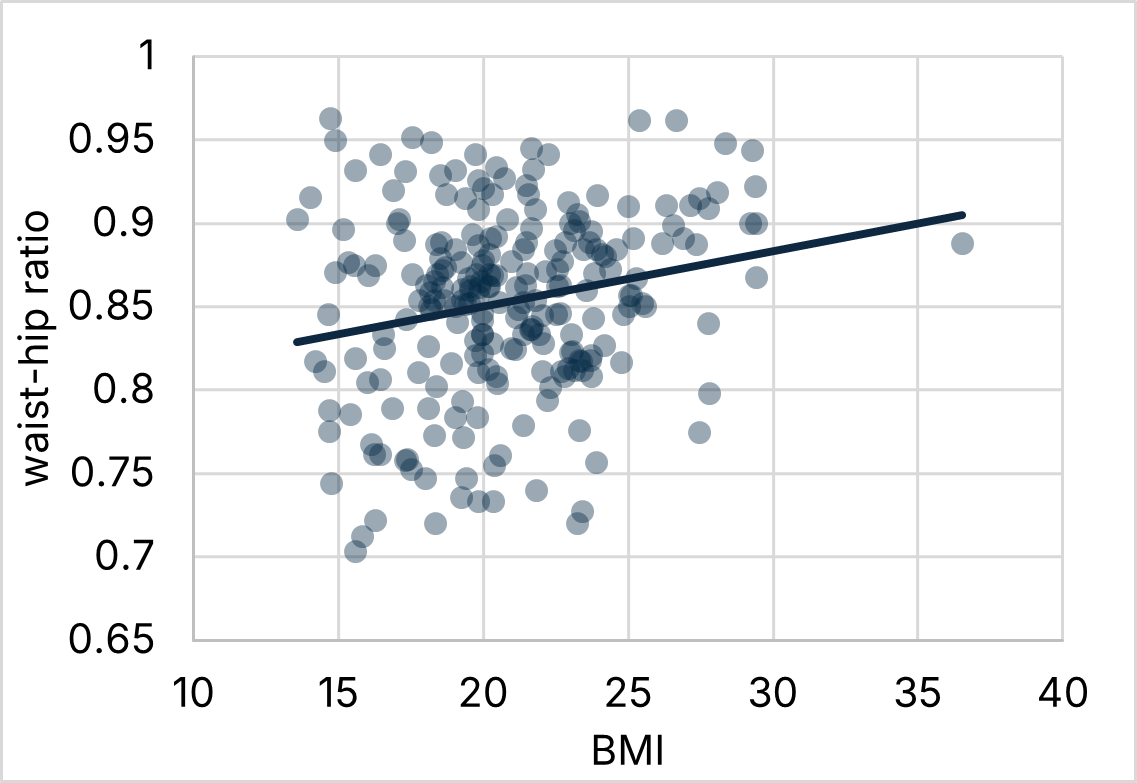
The Pearson’s correlation coefficient (r) was 0.21 (95% CI: 0.08 to 0.33; p = .001) indicated a weak correlation, implying that BMI and WHR assess different aspects of adiposity. (Figure 1)
Discussion
The present study aimed to determine the correlation between Body Mass Index (BMI) and Waist–Hip Ratio (WHR) among first-year medical students. The findings revealed that although the majority of participants had BMI and WHR values within the normal range, a considerable proportion of male students exhibited central obesity based on WHR despite having a normal BMI. This highlights an important limitation of BMI as a solitary measure of adiposity, as it does not differentiate between lean body mass and fat distribution.
The overall prevalence of overweight and obesity based on BMI was modest, with higher rates observed among males than females. Panda et al.[7] reported that the prevalence of overweight and obesity among Indian adolescents ranged from 2.6% to 28.1% in males and 2.7% to 44.5% in females. The difference observed in the present study may be attributed to geographical variation, lifestyle factors, and the relatively smaller sample size.
When classified according to WHR, central obesity was found to be more prevalent among males. Similar findings were reported by Nawab et al.[8], who observed that central obesity (28.5%; 95% CI: 25.2, 32.0) was almost double that of generalised obesity (14.6%; 95% CI: 12.1, 17.6). This difference may be due to variations in fat distribution, dietary patterns, and gender-related physiological differences.
Correlation analysis between BMI and WHR in the present study revealed no significant relationship (r ≈ 0.21), indicating that these two indices assess distinct aspects of body composition. The Kappa statistic (κ = 0.019, SE = 0.076; 95% CI: -0.130, 0.168) demonstrated only slight non-significant agreement between BMI- and WHR-based classifications. Doustjalali et al.[3] also reported similar findings, with no significant correlation between BMI and WHR. This poor concordance reinforces that reliance on BMI alone may underestimate central obesity, which is a more sensitive predictor of metabolic and cardiovascular risk.
Several studies have emphasised that central adiposity, measured through WHR or waist circumference, is more strongly associated with metabolic syndrome and cardiovascular morbidity than general obesity measured by BMI. Therefore, the routine use of both BMI and WHR in screening programmes, especially among young adults and medical students, may help in early identification of individuals at risk of developing non-communicable diseases.
Overall, the findings of the present study suggest that BMI and WHR capture different dimensions of body composition. Hence, both parameters should be considered concurrently when assessing adiposity among young adults to ensure a more comprehensive evaluation of metabolic risk.
Conclusion
The findings of this study indicate a lack of significant correlation and only slight agreement between BMI and WHR classifications among medical students. Both parameters should be used together for comprehensive assessment of adiposity, as WHR identifies central obesity that may be overlooked by BMI alone.
Limitations
The present study was limited by its cross-sectional design, which precludes causal inference. Additionally, the WHR classification has only two categories, which restricts direct comparison with the four BMI categories. Further, the sample was limited to first-year medical students from a single institution, which may limit generalizability.
The relatively low prevalence of obesity in this study population may reflect higher health awareness among medical students; however, lifestyle changes and academic stress can influence future weight gain. Hence, health education and promotion of physical activity should be integrated into medical training programs to prevent obesity and related complications.
Declaration
Conflict of Interest: Author, Dr Margi Sheth is an editor for Journal of Public and Clinical Health Research but was not involved in the editorial review or selection process for this manuscript, which was handled entirely by an independent Guest Editor.
Funding: Nill
References
- Abdelaal M, le Roux CW, Docherty NG. Morbidity and mortality associated with obesity. Ann Transl Med 2017;5(7):161. doi:10.21037/ATM.2017.03.107
- Cercato C, Fonseca FA. Cardiovascular risk and obesity. Diabetology & Metabolic Syndrome 2019 11:1 2019;11(1):1–15. doi:10.1186/S13098-019-0468-0
- Daustalji RS, Gujjar R, Sharma R et al. Correlation between Body Mass Index(BMI) and Waist to Hip Ratio (WHR) among Undergraduate Students. Pakistan Journal of Nutrition 2016;15(7):618–24. doi:10.3923/pjn.2016.618.624
- Verma M, Rajput M, Kishore K, Kathirvel S. Asian BMI criteria are better than WHO criteria in predicting Hypertension: A cross-sectional study from rural India. J Family Med Prim Care 2019;8(6):2095. doi:10.4103/JFMPC.JFMPC_257_19
- WHO. Waist Circumference and Waist–Hip Ratio. WHO Expert 2011;64(1):2–5.
- McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb) 2012;22(3):276. doi:10.11613/bm.2012.031.
- Panda A, Parida J, Jena S, Behera SS, Pradhan A, Patra PK, et al. Prevalence and associated risk factors of overweight and obesity among adolescent population of India: a scoping review. BMC Nutrition 2025 11:1 2025;11(1):1–15. doi:10.1186/S40795-025-01088-0
- Nawab T, Khan Z, Khan IM, Ansari MA. Central obesity is a burden even in normal weight adolescents of a non-metropolitan Indian City: A case for alarm and action for prevention and control. J Family Med Prim Care 2025;14(1):283. doi:10.4103/JFMPC.JFMPC_967_24

