Radiological Evaluation and Clinical Profile of Patients with Miliary Mottling on Chest X-ray: A Cross-Sectional Study
2Professor, Department of Respiratory Medicine, B J Medical College, Ahmedabad, India
3Assistant Professor, Department Community Medicine, GMERS Medical College Himmatnagar, India
Abstract
Introduction: Miliary mottling on chest X-ray refers to diffuse, tiny nodular shadows resembling millet seeds (~2 mm). It is most commonly caused by miliary tuberculosis (TB). This study aims to evaluate the radiological patterns, differential diagnoses, and clinical profiles of patients with miliary mottling. Methods: A prospective observational study was conducted at the Department of Pulmonary Medicine, of one of the tertiary care hospitals of Ahmedabad, over one year (Feb 2022–Jan 2023). Fifty adult patients (>18 years) presenting with miliary mottling on chest X-ray were enrolled based on inclusion/exclusion criteria. All underwent detailed clinical evaluation, laboratory tests, chest imaging (including HRCT when needed), and were followed up daily until discharge or clinical resolution. Data was recorded using a pretested Case Record Form. Results: Among 50 patients, miliary mottling was most common in males (64%) and in the 21–30-year age group (32%). Sputum AFB was positive in only 8%. Crackles were the most frequent respiratory finding (52%), while 42% had no abnormal chest signs. Radiologically, 92% showed classic miliary patterns. Miliary tuberculosis was the predominant cause (86%), with tubercular meningitis as the most common complication (12%). Conclusions: Chest X-ray remains a crucial, cost-effective initial diagnostic tool. HRCT adds specificity by classifying nodule patterns and aiding in differential diagnosis. Early identification of the etiology helps guide timely treatment.
Keywords: HRCT, Miliary Mottling, Miliary Tuberculosis, Pulmonary Nodules
Introduction
Miliary mottling refers to a distinct radiographic pattern characterized by diffuse, small (approximately 1–3 mm), discrete nodules scattered throughout the lung fields, resembling millet seeds-hence the term “miliary.” This pattern, although not disease-specific, is classically associated with miliary tuberculosis (TB), a form of disseminated TB resulting from hematogenous spread of Mycobacterium tuberculosis. However, a variety of infectious, neoplastic, and inflammatory conditions can also present with a similar radiological appearance.[1]
The most frequent and clinically significant cause of miliary mottling in regions with high TB prevalence is miliary tuberculosis, especially among pediatric and immunocompromised populations. Miliary nodules suggest either a compromised immune response to an infectious organism or a diffuse infiltrative disease that spreads through the pulmonary interstitium. The radiological pattern represents lymphohematogenous spread, making it a crucial clue in early diagnosis and management of potentially life-threatening conditions.[2]
Chest radiography remains one of the most accessible and cost-effective tools in the initial assessment of patients with respiratory complaints. However, the sensitivity of conventional chest X-rays for detecting early or subtle miliary patterns may be limited. High-resolution computed tomography (HRCT), particularly with 1–2 mm slice thickness, greatly enhances visualization of the lung parenchyma and aids in identifying the distribution and morphology of nodules, thereby narrowing the differential diagnosis. HRCT can categorize nodular patterns into centrilobular, random, and perilymphatic distributions, which helps guide clinicians toward a more focused diagnostic approach.[3–5] Early differentiation between infectious and non-infectious causes is critical for timely intervention and improved outcomes.[6]
The primary aim of this study is to evaluate the diagnostic significance of chest radiography in detecting miliary mottling and to underscore the value of HRCT in further characterizing such patterns. The study also seeks to identify and analyse the various etiologies of miliary mottling, describe their radiological presentations, and examine complications associated specifically with miliary tuberculosis. By addressing these objectives, the study aims to contribute to more accurate and timely diagnoses, thereby informing clinical decisions and improving patient care.
Methods
This cross-sectional study was conducted in the Department of Pulmonary Medicine at one of the tertiary care hospitals of Ahmedabad, over a period of one year from February 2022 to January 2023. Total 50 participants were selected by convenient sampling technique. The study included patients above 18 years of age, of either sex, who had chest radiographs suggestive of miliary mottling and who provided written informed consent. Patients were excluded if they had nodular opacities inconsistent with a miliary pattern, or were uncooperative or agitated, making clinical evaluation unreliable.
All enrolled patients underwent a thorough evaluation that included detailed history taking, physical examination, and a comprehensive battery of investigations. The diagnostic workup comprised hematological tests, sputum microscopy for acid-fast bacilli (AFB), cartridge-based nucleic acid amplification test (CBNAAT), blood and sputum cultures. TB was confirmed based on a positive CBNAAT result for Mycobacterium tuberculosis. Selected cases also underwent bronchoscopy and pleural fluid analysis where clinically appropriate. Clinical and investigative data were recorded using a pre-validated Case Record Form to ensure consistency and accuracy.
The study protocol was reviewed and approved by the Institutional Ethics Committee. Informed written consent was obtained from all participants.
Statistical analysis was performed in which categorical variables were presented as frequencies and percentages.
Results
A total of 50 patients with radiologically confirmed miliary mottling on chest X-ray were included in this study. The demographic and clinical characteristics, radiographic patterns, systemic findings, complications, and underlying causes were analysed in detail.
The study revealed notable demographic and clinical characteristics among patients with miliary mottling on chest X-ray (Table 1). A clear male predominance was observed, with 64% of the patients being male, compared to 36% female. The age distribution showed the highest incidence in the third decade (21–30 years), accounting for 32% of cases, followed by the fifth decade (41–50 years) at 28%, and the fourth decade (31–40 years) at 24%. The incidence declined with advancing age, with only 14% in the sixth decade and 2% above 60 years.
| Category | No. of Patients, n (%) |
|---|---|
| Sex Distribution | |
| Male | 32 (64.0%) |
| Female | 18 (36.0%) |
| Age Distribution | |
| 21–30 years | 16 (32.0%) |
| 31–40 years | 12 (24.0%) |
| 41–50 years | 14 (28.0%) |
| 51–60 years | 7 (14.0%) |
| >61 years | 1 (2.0%) |
| Habits | |
| Smokers | 15 (30.0%) |
| Tobacco Chewers | 5 (10.0%) |
| Alcoholics | 2 (4.0%) |
| No Habits | 28 (56.0%) |
| Sputum AFB Result | |
| Positive | 4 (8.0%) |
| Negative | 46 (92.0%) |
Regarding lifestyle habits, 30% of the patients were smokers, 10% were tobacco chewers, and 4% reported alcohol consumption. More than half of the patients (56%) had no identifiable substance use history. These findings suggest that while certain habits may contribute to respiratory vulnerability, a significant proportion of patients developed miliary mottling in the absence of such risk factors.
In terms of microbiological confirmation, sputum AFB positivity was low, with only 8% testing positive, while 92% were AFB-negative. This underscores the diagnostic limitation of sputum smear microscopy in cases of miliary tuberculosis, emphasizing the need for radiological and clinical correlation in such presentations.
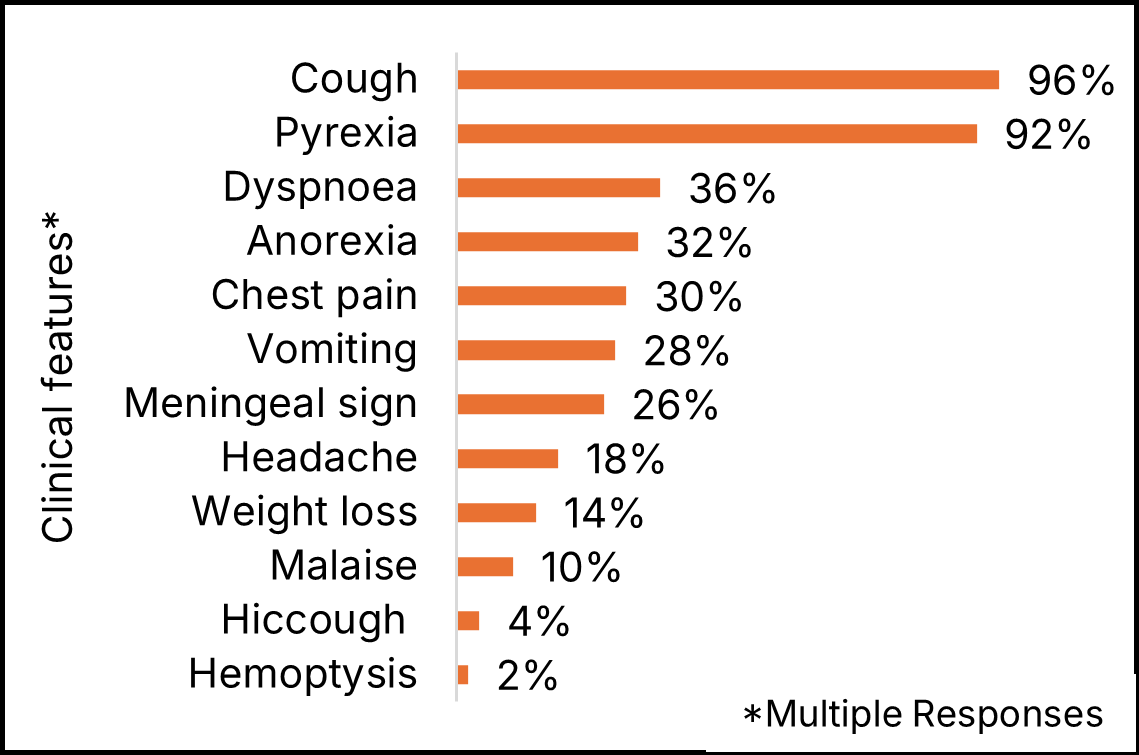
Graph shows that the most common presenting symptoms among patients in this study were cough (96%) and pyrexia (92%). Other frequently observed symptoms included dyspnoea (36%), chest pain (30%), anorexia (32%), vomiting (28%), headache (18%), and weight loss (14%). Meningeal signs such as neck rigidity and a positive Kernig’s sign were noted in 26% of patients. Hemoptysis was observed in one patient.
| Category | No. of Patients, n (%) |
|---|---|
| G/E Findings | |
| Anaemia | 33 (66.0%) |
| Jaundice | 3 (6.0%) |
| Systemic Examination | |
| Crackles | 26 (52.0%) |
| Clinically NAD (Normal) | 21 (42.0%) |
| Signs of Pleural Effusion | 2 (4.0%) |
| Signs of Pneumothorax | 1 (2.0%) |
| CNS Signs | |
| Neck Rigidity | 5 (10.0%) |
| Kernig’s Sign | 2 (4.0%) |
| Abdominal Signs | |
| Hepatomegaly | 4 (8.0%) |
| Chest X-ray (P-A) Findings | |
| Miliary mottling | 46 (92.0%) |
| Miliary + Pleural Effusion | 2 (4.0%) |
| Miliary + Cardiomegaly | 1 (2.0%) |
| Miliary + Pneumothorax | 1 (2.0%) |
| Complications | |
| Tubercular Meningitis (TBM) | 6 (12.0%) |
| Acute Renal Failure (ARF) | 3 (6.0%) |
| Pleural Effusion | 2 (4.0%) |
| Acute Respiratory Distress Syndrome (ARDS) | 2 (4.0%) |
| Congestive Heart Failure (CHF) | 1 (2.0%) |
| Pneumothorax | 1 (2.0%) |
| Causes of Miliary Mottling | |
| Miliary Tuberculosis | 43 (86.0%) |
| Pneumoconiosis | 5 (10.0%) |
| Sarcoidosis | 1 (2.0%) |
| Metastasis | 1 (2.0%) |
The study highlighted a range of clinical, radiological, and etiological findings in patients with miliary mottling on chest X-ray (Table 2). Respiratory examination revealed crackles in 52% of patients, while 42% had no detectable abnormality. CNS signs such as neck rigidity and Kernig’s sign were seen in 10% and 4% of patients, respectively. Hepatomegaly was present in 8%.
Radiologically, isolated miliary mottling was observed in 92% of cases. Additional findings included pleural effusion (4%), cardiomegaly (2%), and pneumothorax (2%). The most common complication was tubercular meningitis (12%), followed by acute renal failure (6%), pleural effusion and ARDS (4% each), and isolated cases of CHF and pneumothorax.
Miliary tuberculosis accounted for the majority of cases (86%), while pneumoconiosis (10%), sarcoidosis (2%), and metastasis (2%) were less common causes.
Discussion
This study aimed to evaluate the clinical, radiological, and laboratory profiles of patients with miliary tuberculosis and to compare these findings with other relevant studies. The results underscore several important patterns in the presentation and complications of miliary tuberculosis, with implications for early diagnosis and management. The most common radiological finding in this study was miliary mottling on chest X-ray, observed in 92% of patients, reinforcing its central role in diagnosing disseminated tuberculosis. This incidence was higher than that reported by Proudfoot et al.[7] (58.3%), possibly reflecting improved imaging access or more severe disease at presentation in study setting.
Cough (96%) and pyrexia (92%) were the most frequently reported symptoms, consistent with findings from Gelb et al.[8] and Abakay et al.[9], although with higher prevalence in the present study. These symptoms remain critical early indicators, especially in endemic regions. Notably, meningeal signs were observed in 26%, emphasizing the importance of CNS evaluation in suspected cases. This was also highlighted in studies by Proudfoot et al.[7], who reported a TBM prevalence of 17%.
Demographically, the present study found the highest incidence of miliary TB among individuals aged 21–50 years, particularly in the 21–30 age group (32%). This differs from Proudfoot et al.[7], who noted a peak incidence in older adults. These variations may reflect differing population demographics, host immunity, or exposure risks.
A notable systemic finding was anaemia in 66% of patients, aligning with Abakay et al.[9] This could be attributed to chronic disease, nutritional deficiency, or bone marrow involvement. Hepatomegaly was noted in 8% and pleural effusion in 4%, lower than rates reported in Gelb AF et al.[8] study, suggesting possible differences in disease severity or co-infections. Compared to Gelb AF et al.[8] and Abakay O et al.[9], this study shows a higher burden of respiratory symptoms and radiographic abnormalities. These differences may stem from diagnostic delays or more advanced disease stages at presentation. While Proudfoot et al.[7] observed higher rates of complications such as TBM and other systemic manifestations, present study did not identify complications like DVT or GI bleeding, which may reflect sample size or selection bias.
Gender distribution revealed a male predominance (64%), which aligns with Gelb AF et al.[8] and Proudfoot et al.[7] This could be linked to gender-related exposure differences, healthcare access, or immunological factors.
Limitations
This study was conducted at a single tertiary care centre and had a small sample size, which may limit the findings' generalisability. Furthermore, no long-term follow-up was carried out, making it hard to assess treatment outcomes and late complications. Selection bias from convenience sampling could also have influenced the results.
Conclusion
Miliary mottling on chest X-ray should raise clinical suspicion for miliary TB but warrants comprehensive evaluation to confirm diagnosis. HRCT is indispensable for pattern recognition and aids in narrowing differentials, guiding appropriate therapy.
Declaration
Conflict of Interest: None
Funding: Nill
References
- Vohra S, Dhaliwal HS. Miliary Tuberculosis. Treasure Island (FL): StatPearls Publishing; 2024
- Alende-Castro V, Macía-Rodríguez C, Páez-Guillán E, García-Villafranca A. Miliary pattern, a classic pulmonary finding of tuberculosis disease. J Clin Tuberc Other Mycobact Dis 2020;20:100179. doi:10.1016/j.jctube.2020.100179
- Ghodrati S, Pugashetti J V, Kadoch MA, Ghasemiesfe A, Oldham JM. Diagnostic Accuracy of Chest Radiography for Detecting Fibrotic Interstitial Lung Disease. Ann Am Thorac Soc 2022;19(11):1934–7. doi:10.1513/AnnalsATS.202112-1377RL
- Bhalla AS, Goyal A, Guleria R, Gupta AK. Chest tuberculosis: Radiological review and imaging recommendations. Indian J Radiol Imaging 2015;25(3):213–25. doi:10.4103/0971-3026.161431.
- Klein JS, Rosado-de-Christenson ML. A Systematic Approach to Chest Radiographic Analysis. In: Hodler J, Kubik-Huch RA, von Schulthess GK, editors. Dis. Chest, Breast, Hear. Vessel. 2019-2022 Diagnostic Interv. Imaging, Cham (CH): Springer; 2019. Chapter 1. doi:10.1007/978-3-030-11149-6_1
- Sharma SK, Mohan A, Sharma A. Challenges in the diagnosis \& treatment of miliary tuberculosis. Indian J Med Res 2012;135(5):703–30
- Proudfoot AT, Akhtar AJ, Douglas AC, Horne NW. Miliary tuberculosis in adults. Br Med J 1969;2(5652):273–6. doi:10.1136/bmj.2.5652.273
- Gelb AF, Lefler C, Brewin A, Mascatello V, Lyons H. Miliary tuberculosis. Am Rev Respir Dis 1973;108(6):1327-33. doi:10.1164/arrd.1973.108.6.1327
- Abakay O, Abakay A, Tanriverdi H, Selimoğlu Sen H, Sezgi C, Kaya H, et al. Clinical and laboratory characteristics of 48 patients with miliary tuberculosis. African J Microbiol Res 2011;5(29):5292–6. doi: 10.5897/AJMR11.644
