Trends in New Case Detection and Epidemiological Patterns of Leprosy in Vadodara District, Gujarat: A Three-Year Descriptive Study (2019-2022)
2Assistant Professor, Department of Community Medicine, Government Medical College, Vadodara, India
3Additional District Health Officer, Vadodara, India
4In charge District Leprosy Officer, Vadodara, India
Abstract
Introduction: Despite achieving elimination status at the national level, leprosy continues to exhibit regional disparities in India. Vadodara district reported an annual new case detection rate (ANCDR) of 6.09 per 100,000 population in 2021-22, indicating persistent transmission. This study aimed to analyse the three-year trends (2019-2022) in leprosy case detection and assess epidemiological patterns to inform targeted interventions. Methods: A descriptive temporal trend analysis was conducted using secondary data from the District Leprosy Office, Vadodara. Data were extracted from offline hard-copy registers, digitized into Microsoft Excel, and analysed for the three-year trends (2019-2022) in case detection, demographic distribution, and key leprosy indicators. The study assessed ten administrative blocks within the district. Results: A declining trend in new leprosy cases was observed across most blocks, except Sinor, which reported a continuous increase. Female cases constituted 40.6% of total cases, while 23 child cases (age <15 years) were detected over the study period. Multibacillary (MB) leprosy accounted for 73.42% of adult cases, whereas paucibacillary (PB) cases were more common in children. All leprosy indicators-ANCDR, child proportion, female proportion, MB proportion, and deformity proportion-showed a gradual annual decline. Conclusion: The study highlights a decreasing trend in leprosy cases in Vadodara district, suggesting progress toward elimination. However, persistent regional disparities, particularly in Sinor block, necessitate targeted surveillance and intervention strategies.
Keywords: Epidemiology, Leprosy, Vadodara
Introduction
Leprosy, caused by Mycobacterium leprae, remains a public health challenge in India despite the country achieving national elimination (defined as a prevalence rate below 1 case per 10,000 population) in 2005.[1] However, elimination does not equate to eradication, as localized hotspots with active transmission persist, underscoring the need for sustained surveillance and targeted interventions. One such region is Gujarat, where Vadodara district reported an annual new case detection rate (ANCDR) of 6.09 per 100,000 population in 2021–22, signalling ongoing transmission. Monitoring these trends is critical to identifying high-risk areas and refining elimination strategies. This study aimed to (1) describe the three-year trend (2019–2022) in new case detection, (2) analyse the geographical and demographic distribution of cases, and (3) assess key leprosy indicators-including ANCDR, child proportion, female proportion, multibacillary (MB) proportion, and deformity proportion. By doing so, the findings will help prioritize high-risk populations and guide focused interventions to accelerate progress toward sustained elimination.
Methods
This was a descriptive temporal trend analysis of leprosy cases reported in Vadodara district, Gujarat, over three years (April 2019 to March 2022). The district is administratively divided into 10 blocks for leprosy surveillance and reporting. Data were obtained from offline hard-copy registers maintained at the District Leprosy Office, Vadodara. The records included Quarterly case reports (Q1-Q12, representing three-month periods) and Clinical classification (MB, PB, MB-child, PB-child, deformity status). The data were digitized into Microsoft Excel with assistance from the District Leprosy Office’s medical officer and data manager. Digitized records were cross-checked against original registers by the research team and DLO staff to minimize entry errors. Incomplete records (e.g., unspecified clinical classification or missing demographic details) were completed with consulting patients telephonically by DLO staff. Unique identification numbers were used to identify and merge duplicate entries from overlapping quarterly reports.
The study assessed (1) temporal trends (quarterly and annual case detection), (2) geographical distribution across the 10 blocks, (3) demographic patterns (age, sex), and (4) key leprosy indicators: Annual New Case Detection Rate (ANCDR), child proportion (<15 years), female proportion, MB proportion, and deformity proportion (grade 2 disabilities). Quarterly trends were analysed for each fiscal year (2019–20, 2020–21, 2021–22), with descriptive statistics (proportions, medians) summarizing clinical and demographic characteristics. The interquartile range (IQR) was calculated to evaluate case distribution variability across blocks.
This study analysed secondary, anonymized programmatic data obtained from the District Leprosy Office (DLO), Vadodara, with official permission from the DLO authorities. As per ICMR National Ethical Guidelines (2017, Section 8.3 and table 4.1, sr.no 1: Exemption from review) ethical committee approval was not required.[2] Patient records were anonymized, and data were stored in password-protected files.
Results
This study analysed 719 cases of Leprosy. The graph (Figure 1) illustrates significant fluctuations in annually new leprosy case numbers across Vadodara district's administrative blocks over three fiscal years. Parul/Dhiraj, serving as a major institutional catchment zone, consistently reported the district's highest caseloads, accounting for 20-25% of Vadodara's total cases annually. The Corporation area follows as a stable secondary hotspot, demonstrating gradual improvement (51 cases in 2019-20 to 43 cases in 2021-22) yet requiring continued intensive intervention.
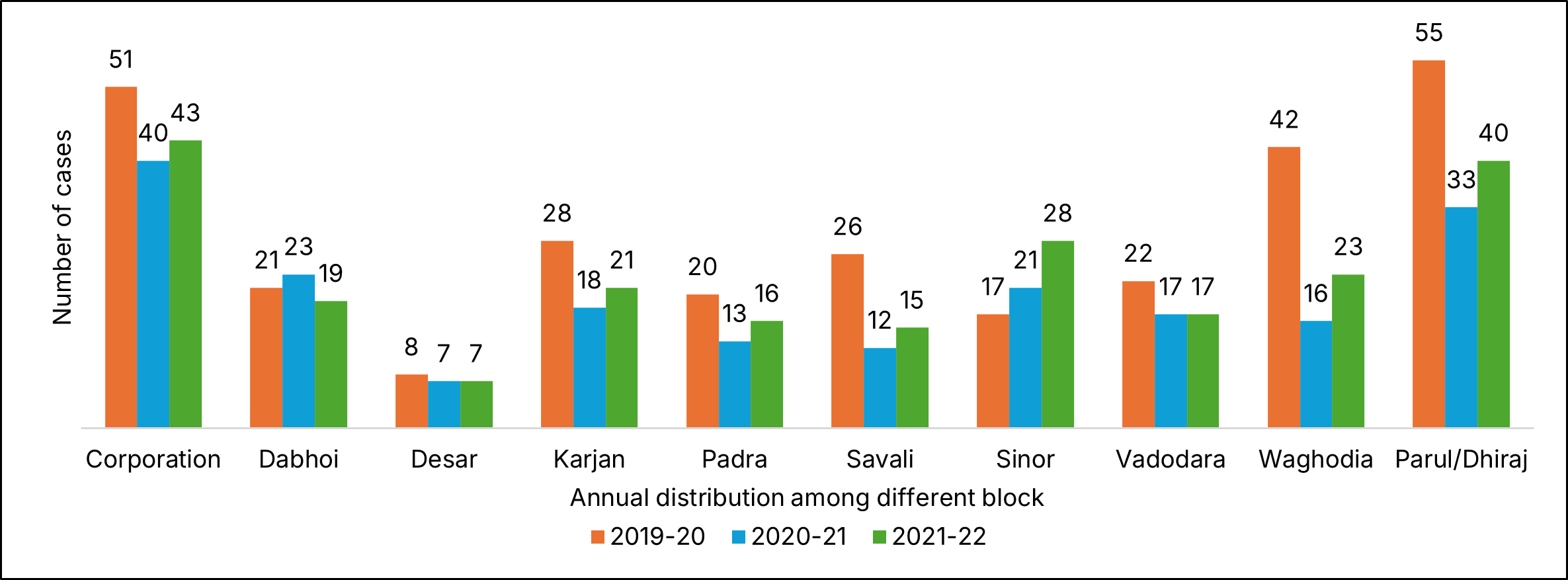
Of particular concern is Sinor block's marked epidemiological shift, exhibiting a 64.7% case increase over three years (from 17 to 28 cases) - the most pronounced upward trajectory district-wide. This trend may indicate either emerging transmission foci or breakdowns in case detection and management systems. In contrast, multiple blocks demonstrate successful control measures, with Waghodia showing the most dramatic reduction (61.9% decrease from peak) and Savali achieving consistent declines (53.8% reduction).
| Baseline characteristic | 2019–20 | 2020–21 | 2021–22 | Total | Median (IQR) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | |||
| Blocks | ||||||||||||||
| Corporation | 21 | 11 | 7 | 12 | 8 | 10 | 9 | 13 | 11 | 13 | 12 | 7 | 134 | 11 (8.75–12.25) |
| Dabhoi | 2 | 9 | 6 | 4 | 6 | 6 | 6 | 5 | 4 | 4 | 6 | 5 | 63 | 5.5 (4–6) |
| Desar | 0 | 6 | 1 | 1 | 1 | 1 | 3 | 2 | 1 | 2 | 3 | 1 | 22 | 1 (1–2.25) |
| Karjan | 7 | 14 | 4 | 3 | 5 | 5 | 5 | 3 | 3 | 6 | 8 | 4 | 67 | 5 (3.75–6.25) |
| Padra | 5 | 5 | 6 | 4 | 2 | 2 | 6 | 3 | 2 | 4 | 6 | 4 | 49 | 4 (2.75–5.25) |
| Savali | 5 | 13 | 4 | 4 | 2 | 4 | 4 | 2 | 3 | 5 | 3 | 4 | 53 | 4 (3–4.25) |
| Sinor | 5 | 4 | 4 | 4 | 3 | 6 | 7 | 5 | 6 | 11 | 5 | 6 | 66 | 5 (4–6) |
| Vadodara | 5 | 12 | 2 | 3 | 2 | 6 | 5 | 4 | 3 | 5 | 4 | 5 | 56 | 4.5 (3–5) |
| Waghodia | 12 | 16 | 8 | 6 | 4 | 4 | 5 | 3 | 3 | 5 | 7 | 8 | 81 | 5.5 (4–8) |
| Parul / Dhiraj | 19 | 12 | 13 | 11 | 10 | 3 | 9 | 11 | 8 | 16 | 12 | 4 | 128 | 11 (8.75–12.25) |
| Gender | ||||||||||||||
| Female | 27 | 51 | 28 | 22 | 18 | 16 | 20 | 17 | 18 | 26 | 26 | 23 | 292 | |
| Male | 54 | 51 | 27 | 30 | 25 | 31 | 39 | 34 | 26 | 45 | 40 | 25 | 427 | |
| Age Group | ||||||||||||||
| <14 Years | 2 | 6 | 3 | 0 | 0 | 2 | 4 | 0 | 1 | 4 | 1 | 0 | 23 | |
| 14–60 Years | 61 | 87 | 43 | 46 | 39 | 41 | 50 | 47 | 38 | 64 | 55 | 39 | 610 | |
| >60 Years | 18 | 9 | 9 | 6 | 4 | 4 | 5 | 4 | 5 | 3 | 10 | 9 | 86 | |
| PB/MB cases | ||||||||||||||
| MB | 61 | 68 | 44 | 43 | 32 | 28 | 40 | 36 | 31 | 47 | 44 | 37 | 511 | |
| MB-C | 1 | 2 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 3 | 0 | 0 | 10 | |
| PB | 18 | 28 | 9 | 9 | 11 | 17 | 15 | 15 | 12 | 20 | 21 | 11 | 186 | |
| PB-C | 1 | 4 | 1 | 0 | 0 | 1 | 3 | 0 | 0 | 1 | 1 | 0 | 12 | |
| Total | 81 | 102 | 55 | 52 | 43 | 47 | 59 | 51 | 44 | 71 | 66 | 48 | 719 | |
Note. Q1 = April to June, Q2 = July to September, Q3 = October to December, Q4 = January to March. MB = Multibacillary, MB-C = Multibacillary child cases, PB = Paucibacillary, PB-C = Paucibacillary child cases.
Demographic analysis (Table 1) showed women accounted for 40.6% of total cases, while 23 pediatric cases (under 15 years) were detected, with paucibacillary (PB) form being more common in children. Notably, 73.42% of adult cases presented as multibacillary (MB), suggesting a significant burden of advanced disease. Two blocks - Desar and Padra - reported no pediatric cases during the entire study period.
| Block | Annually Detected Female Cases | Annually Detected Child Cases | Annually New Detected Cases | Annually Detected MB Cases | Annually Detected Deformity Cases | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2019-20 | 2020-21 | 2021-22 | 2019-20 | 2020-21 | 2021-22 | 2019-20 | 2020-21 | 2021-22 | 2019-20 | 2020-21 | 2021-22 | 2019-20 | 2020-21 | 2021-22 | |
| Corporation | 17 | 13 | 16 | 0 | 1 | 0 | 51 | 40 | 43 | 50 | 38 | 43 | 1 | 1 | 0 |
| Dabhoi | 9 | 10 | 10 | 0 | 1 | 0 | 21 | 23 | 19 | 11 | 13 | 9 | 0 | 0 | 0 |
| Desar | 6 | 2 | 4 | 0 | 0 | 0 | 8 | 7 | 7 | 3 | 3 | 2 | 0 | 0 | 0 |
| Karjan | 11 | 8 | 8 | 4 | 0 | 1 | 28 | 18 | 21 | 21 | 12 | 15 | 0 | 0 | 0 |
| Padra | 10 | 3 | 6 | 0 | 0 | 0 | 20 | 13 | 16 | 16 | 8 | 5 | 1 | 0 | 0 |
| Savali | 16 | 6 | 8 | 1 | 1 | 0 | 26 | 12 | 15 | 17 | 6 | 10 | 0 | 0 | 0 |
| Sinor | 6 | 8 | 16 | 1 | 1 | 2 | 17 | 21 | 28 | 8 | 6 | 13 | 0 | 0 | 0 |
| Vadodara | 10 | 5 | 9 | 2 | 0 | 1 | 22 | 17 | 17 | 13 | 8 | 10 | 0 | 0 | 0 |
| Waghodia | 25 | 9 | 9 | 2 | 2 | 1 | 42 | 16 | 23 | 26 | 11 | 16 | 0 | 0 | 1 |
| Parul/Dhiraj | 18 | 7 | 7 | 1 | 0 | 1 | 55 | 33 | 40 | 55 | 33 | 40 | 0 | 0 | 0 |
| Total | 128 | 71 | 93 | 11 | 6 | 6 | 290 | 200 | 229 | 220 | 138 | 163 | 2 | 1 | 1 |
The study identified significant geographical variations (Table 2) in leprosy case distribution across Vadodara district. Waghodia, Parul, and Dhiraj blocks reported disproportionately fewer female cases, with Parul and Dhiraj's status as institutional catchment areas potentially influencing this gender disparity in reporting. Most notably, Sinor block emerged as a persistent high-burden area, maintaining consistently elevated case numbers that suggest either ongoing transmission or gaps in healthcare access.
| Leprosy Indicators | 2019-20 | 2020-21 | 2021-22 |
|---|---|---|---|
| Female Proportion (Percentage to newly detected total cases) | 44.1 | 35.5 | 40.6 |
| Child Proportion (Percentage to newly detected total cases) | 3.79 | 3 | 2.62 |
| ANCDR (Annually new case detection rate) | 8.03 | 5.44 | 6.09 |
| MB Proportion (Percentage to newly detected total cases) | 75.9 | 69.0 | 71.2 |
| Deformity Proportion (Percentage to newly detected total cases) | 3.79 | 3 | 2.62 |
The analysis of annual leprosy indicators (Table 3) reveals several noteworthy patterns in disease epidemiology across Vadodara district. Female representation among new cases showed significant fluctuation, declined from 44.1% in 2019-20 to 40.6% in 2021-22. More encouraging trends emerged in pediatric cases and disability rates. The proportion of child cases (<15 years) demonstrated consistent annual declines from 3.79% to 2.62%, with deformity proportions mirroring this exact downward trajectory (3.79% to 2.62%). This parallel improvement likely reflects enhanced early detection and treatment initiatives. Case detection patterns revealed pandemic-related impacts, with the ANCDR dropping from 8.03 to 5.44 per 100,000 between 2019-20 and 2020-21 before rebounding to 6.09 in 2021-22. Disease severity indicators showed mixed results - while MB cases decreased from 75.9% to 69% during the first two years, they rose slightly to 71.2% in the final year.
Discussion
This study analysed trends in leprosy case detection and epidemiological patterns in Vadodara district, Gujarat, from 2019 to 2022. A declining trend in new cases was observed across most administrative blocks, except Sinor, which reported a continuous increase. Females constituted 40.6% of total cases, while 23 paediatric cases (<15 years) were detected. Multibacillary (MB) leprosy accounted for 73.42% of adult cases, whereas paucibacillary (PB) cases were more common in children. Key indicators-annual new case detection rate (ANCDR), child proportion, female proportion, MB proportion, and deformity proportion-showed a gradual annual decline.
Key Findings:
- High MB Rates in Adults: The predominance of MB cases (73.42%) suggests delayed diagnosis or prolonged transmission. Similar findings were reported in West Bengal, where diagnostic delays (≥90 days) significantly increased the odds of MB leprosy (adjusted OR = 2.75).[3] Misclassification and late detection due to clinical overlap with other dermatological conditions further exacerbate this issue, as observed in Maharashtra’s leprosy case detection campaigns.[4]
- PB Predominance in Children: The higher proportion of PB cases in children may reflect recent transmission or differences in immune response. Children’s developing immune systems may better control bacterial proliferation, leading to milder presentations. Alternatively, early detection through school-based surveillance or familial contact tracing could explain this trend, as seen in tribal populations where pediatric cases are often underreported.[5]
- Sinor Block’s Rising Trend: Sinor block exhibited a 64.7% increase in cases, contrasting with declines elsewhere. Possible explanations include:
- Migration: Influx from endemic regions, as observed in Kerala’s tribal communities, introduces new infections.[5]
- Active Case Detection: Improved surveillance may uncover previously undetected cases, similar to Maharashtra’s LCDCs.[4]
- Awareness Gaps: Low community knowledge and stigma delay reporting, as noted in West Bengal, where 51% of MB cases attributed delays to "not perceiving symptoms seriously".[3]
- Post-Pandemic Case Increase (2021–22): The rebound in cases (ANCDR: 5.44 to 6.09) after the 2020–21 dip likely reflects disrupted healthcare access during COVID-19, followed by catch-up detection. Underreporting and misclassification during the pandemic were also reported in Maharashtra, where active case detection revealed hidden burdens.[4]
- Strengthening Early Diagnosis and Surveillance:
- Enhanced Training: Healthcare workers should be trained to differentiate MB from PB cases early, leveraging molecular diagnostics where feasible.[6]
- Active Case Detection: Quarterly screenings, as opposed to annual surveys, can reduce diagnostic delays, particularly in high-burden areas like Sinor.[3]
- Targeted Interventions for High-Risk Groups:
- Community Awareness: Campaigns should focus on high-risk populations (e.g., married males, migrants) to reduce stigma and promote early care-seeking.[3]
- Pediatric Surveillance: Integrate leprosy screening with routine child health programs to improve early detection.[5]
- Resilient Health Systems:
- Integration with Primary Healthcare: Embed leprosy surveillance within general health services to mitigate disruptions, as recommended in the National Strategic Plan 2023–2027.[6]
- Data Audits: Regular reviews of case registers and use of eHealth tools can minimize misclassification and improve real-time monitoring.[6]
Conclusion
While Vadodara district shows progress, MB predominance, pediatric PB cases, and Sinor’s outlier status demand tailored interventions. Strengthening surveillance, addressing diagnostic delays, and targeting high-risk populations will be pivotal for sustained elimination. The findings align with national priorities, such as the National Strategic Plan 2023–2027, which emphasizes early detection, stigma reduction, and equitable access. Future studies should explore sociodemographic determinants of transmission and the impact of migration on localized trends.
Limitations
When interpreting the results, it is important to take into account the significant limitations of this study. First, the use of secondary data from district health registers might have resulted in biases in the recording of cases and insufficient information about them, especially when it came to clinical classifications and demographics. Second, the three-year study period (2019–2022) might not be long enough to record seasonal fluctuations in leprosy transmission and long-term epidemiological trends. Lastly, the results cannot be applied to other areas with distinct healthcare systems and sociodemographic due to the narrow focus on a single district. These drawbacks emphasise the necessity of additional research that includes multi-site comparisons, primary data collection, and longer observation times.
Acknowledgements
We extend our gratitude to District Leprosy Office, Vadodara, for facilitating data access. We also acknowledge Dr. Jivraj Damor (Professor and Head), Medical College Vadodara, India for their guidance.
Declaration
Conflict of Interest: None
Funding: Nill
References
- Park K. Park’s Textbook of Preventive and Social Medicine. 27th ed. Jabalpur: M/S Banarsidas Bhanot Publishers; 2023.
- Mathur R, Swaminathan S. National ethical guidelines for biomedical and health research involving human participants. New Delhi: Director-General, Indian Council of Medical Research; 2017.
- Mukhopadhyay DK, Sarkar TK, Chatterjee S, Ray S, Roy P, Biswas AK. Factors Associated with High Prevalence of Multibacillary Leprosy in West Bengal: A Case–Control Study. Indian J Public Health 2024;68(2):157–62. doi:10.4103/ijph.ijph_1004_23.
- Surywanshi SP, Lokhande GS. Clinico Epidemiological Profile of New Leprosy Cases Detected in Leprosy Case Detection Campaign in North Maharashtra during 2018–2020. Indian J Public Health 2023;67(1):152–4. doi:10.4103/IJPH.IJPH_387_22
- Simi SM, Jose R, Anish TS. Skin diseases among the tribal population of Kerala: the challenges and way forward. Int J Equity Health 2024;23(1):172. doi:10.1186/s12939-024-02237-w.
- Katoch VM. Eradication of leprosy from India: Reflections on past, present & future. Indian Journal of Medical Research 2024;159(1):1–5. doi:10.4103/IJMR.IJMR_64_24
