A Cross-Sectional Study on Effect of Serum Potassium Level on Clinical Profile and Outcome in Organophosphorus Poisoning
Abstract
Introduction: Organophosphorus (OP) compounds are commonly used as toxic agents due to their easy availability and low cost. The rising mortality in OP poisoning cases is influenced by multiple factors, one of which is hypokalaemia. This study was conducted to evaluate the outcomes of OP poisoning and examine its relationship with potassium levels. Method: A cross-sectional study was conducted at the tertiary care hospital in Central Gujarat. All the patients above the age of 12 years admitted to the emergency department during the study period were included in the study. Peradeniya Organophosphorus poisoning scale (POP) was used to categorise the severity of the cases. Association was observed between outcome with potassium level and other relevant clinical parameters with appropriate statistical test. p-value less 0.05 was considered as statistically significant. Result: A study of 100 patients found that most (97%) consumed organophosphates (OP) in suicide attempts, with monocrotophos being the most common (28%). Over half were aged 19–45, and two-thirds were male. Only 33% arrived directly from home, while others were referred from healthcare facilities. Vomiting (78%) was the most frequent symptom, and most arrived within eight hours. Based on the POP score, 68% had mild poisoning. While 76 recovered, 34 needed ventilators, and 24 died. Hypokalaemia (56%) was significantly associated with outcomes such as recovered vs dead and no of patients required ventilatory support. Conclusion: Hypokalaemia at the time of presentation has detrimental effect on clinical outcome as it increases requirement of ventilator support.
Keywords: Hypokalaemia, Organophosphorus Poisoning, Peradeniya Organophosphorus Poisoning Scale
Introduction
Organophosphorus (OP) compounds are among the most used pesticides in India, leading to a high incidence of poisoning due to their easy availability.[1] Deliberate self-poisoning with OP pesticides has emerged as a significant public health concern, with both suicidal and accidental exposures contributing to morbidity and mortality. OP compounds, while employed in farming, have also been deployed as chemical weapons, highlighting their dangerous toxic effects.[2] The World Health Organization (WHO) estimates that approximately 3 million cases of pesticide poisoning occur globally each year, resulting in over 220,000 deaths, with the incidence continuing to rise.[3,4]
The toxic effects of OP compounds primarily stem from the inhibition of acetylcholinesterase, leading to excessive accumulation of acetylcholine at neural synapses. This results in a range of cholinergic symptoms, primarily affecting the peripheral nervous system.[5,6] Symptoms typically manifest within 30 to 90 minutes post-ingestion, with some highly lipophilic compounds exhibiting delayed toxicity up to 24 hours due to metabolic bioactivation.[7] The classic mnemonic "SLUDGE" (salivation, lacrimation, urination, defecation, gastrointestinal distress, and emesis) is often used to describe the hallmark symptoms of OP poisoning. While cholinesterase inhibition is central to toxicity, individual susceptibility, inhibition of other enzymatic systems, and direct tissue effects also contribute to the clinical presentation.[6]
Respiratory failure remains the leading cause of mortality in OP poisoning, often resulting from a combination of respiratory muscle weakness and central respiratory depression. Early identification and timely initiation of ventilatory support are crucial in improving survival outcomes.[8,9] Electrolyte disturbances, especially hypokalaemia, are commonly observed in acute cases and contribute to muscle weakness, thereby worsening respiratory failure.[8] The etiology of hypokalaemia is multifactorial, and it is now recognized as a key factor that amplifies the toxic manifestations of OP poisoning.
Given the widespread use of OP compounds in agriculture and industry, their accessibility and affordability continue to pose a significant health hazard. Recognizing the full spectrum of clinical manifestations is essential for timely intervention. Risk stratification, early diagnosis, and prompt management play a crucial role in improving patient outcomes. Therefore, the present study has been conducted to clinically assess and categorize OP poisoning cases on admission using the Peradeniya Organophosphorus Poisoning (POP) scale and determine its correlation with serum potassium levels. Furthermore, the correlation between serum potassium levels and the severity as well as the outcome of acute OP poisoning had been assessed in the study.
Methods
A cross-sectional study was conducted among the patients of Organophosphorus poisoning admitted to the tertiary care hospital of the central Gujarat.
All the patients during the study period (January’ 2023-October’ 2023) were recruited in the study. All patients aged above 12 years with acute organophosphate poisoning admitted to the Medicine Department of the tertiary care hospital within 24 hours of ingestion were included in the study.
Following patients were excluded from the study.
1. Chronic renal disease, epilepsy, known psychiatric illness, myocardial infarction, myocarditis, malignancy or overwhelming sepsis
2. History of respiratory diseases including bronchial asthma, cardiac diseases, neuromuscular diseases like myasthenia gravis or muscular dystrophy or any myopathy
3. Trauma, recent intramuscular injections, burns
4. Dual insecticide/ multiple poisoning with other drugs such as opioids, diazepam, barbiturate etc.
5. All conditions causing of hypokalaemia alkalosis like diuretic use, beta agonist use, high aldosterone levels, insulin overdose, laxative abuse, corticosteroid
The patients were enrolled after taking approval from the Institutional Ethics Committee (IECHR/074-22). An informed written consent was taken from each patient for obtaining medical history, clinical examination and for permission to take blood samples for laboratory investigations. All results obtained from patients were registered in excel sheets and analysed using SPSS software.
Operational Definition:
Acute Case of Organophosphorus Poisoning: OP poisoning was diagnosed clinically based on History or evidence of exposure to anticholinesterase agents, Signs and symptoms of poisoning, blood investigations.
Peradeniya Organophosphorus poisoning scale (POP):[10] POP scale screening should be done as soon as the patient is admitted and before starting any treatment. It helps in assessing the cholinergic effects. The parameters used are respiratory rate, heart rate, pupil size, fasciculations, seizure and level of consciousness. It can be graded as mild 0-3; moderate: 4-7 and severe: 8-11.
Procedure following admission:
Biochemical analysis, including serum potassium estimation and routine investigations, was performed upon admission to assess the severity of poisoning.
1. Estimation of serum and RBC cholinesterase
2. Blood sugar and urine ketones
3. Serum electrolytes, creatinine, bilirubin, liver enzymes
4. CBC
5. Arterial blood gas analysis
6. ECG
7. Chest X-ray
8. Ultrasound scan of the abdomen (pancreatic status).
Samples were collected by a single prick after initial resuscitation and stabilization of patient, from a peripheral vein without tying any tourniquet, nor adding any anticoagulants. Biochemical levels were estimated photometrically using the CHO-POD kinetic photometric test.
Potassium level was estimated using ISE-Direct optimized method. Reference values [3.5-5.1 mg/dL in male and females].
Results
A total of 100 patients were included in the study, with more than half belonging to the 19–45 age group. Nearly two-thirds of the patients were male, and detailed socio-demographic data can be found in Table 1. The majority (97%) had consumed an organophosphate (OP) compound in an attempt to commit suicide. Only 33% of the patients arrived directly from home, while the rest were referred from various healthcare facilities, including Primary Health Centres (25%), Community Health Centres (22%), District Hospitals (12%), and Private Hospitals (8%). Their clinical history is detailed in Table 2.
| Variable | Frequency (%) |
|---|---|
| Age group | |
| 12 – 18 | 09 (09%) |
| 19 – 45 | 56 (56%) |
| 46 – 65 | 29 (29%) |
| >65 | 06 (06%) |
| Gender | |
| Male | 77 (77%) |
| Female | 23 (23%) |
| Occupations | |
| Agricultural labourer | 47 (47%) |
| Construction worker | 31 (31%) |
| Housewife | 09 (09%) |
| Student | 08 (08%) |
| Unemployed | 03 (03%) |
| Business | 02 (02%) |
| History of Addiction | |
| Yes | 82 (82%) |
| No | 18 (18%) |
| Variable | Frequency (%) |
|---|---|
| Symptoms* | |
| Vomiting | 78 |
| Dizziness | 50 |
| Difficulty in breathing | 14 |
| Loss of consciousness | 12 |
| Convulsion | 10 |
| Admission following ingestion of compound (in hours) | |
| ≤4 | 26 |
| 5 to 8 | 42 |
| 9 to 12 | 20 |
| 13 to 16 | 03 |
| 17 to 20 | 06 |
| 21 to 24 | 03 |
| POP score | |
| Mild | 68 |
| Moderate | 20 |
| Severe | 12 |
| Potassium Level | |
| Hypokalaemia | 56 |
| Normal K⁺ | 44 |
| S. AchE | |
| Mild | 94 |
| Moderate | 06 |
| Severe | 00 |
| Need for Ventilator | |
| Yes | 34 |
| No | 66 |
Note. *Multiple answers possible.
| Variable | Potassium Level | p* | |
|---|---|---|---|
| Hypokalaemia | Normal Potassium | ||
| Ventilator Support | |||
| Yes | 31 | 25 | <.001 |
| No | 25 | 41 | |
| Outcome | |||
| Death | 22 | 02 | <.001 |
| Discharge | 34 | 42 | |
| Total | 56 | 44 | |
Note. *Chi-square test.
| Variable | Pearson correlation (r) | p |
|---|---|---|
| Age | 0.088 | .384 |
| RBS | 0.24 | .018 |
| Creatinine | 0.0005 | .996 |
| S. Na⁺ | -0.032 | .754 |
| S. AchE | 0.208 | .038 |
| Hb | 0.050 | .620 |
| TLC | -0.008 | .934 |
| PC | 0.286 | .004 |
| MAP | 0.135 | .181 |
| POP Score | -0.330 | .001 |
Note. RBS = Random Blood Sugar; S. AchE = Serum Acetylcholinesterase; Hb = Haemoglobin; TLC = Total Leucocyte Count; PC = Platelet Count; MAP = Mean Arterial Pressure.
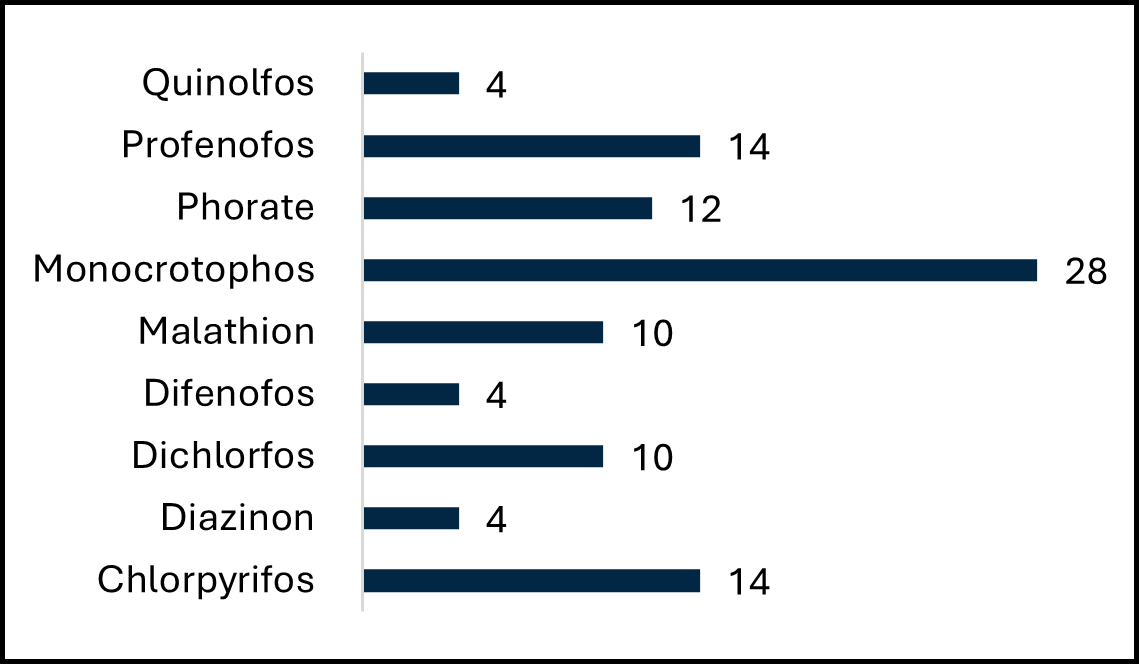
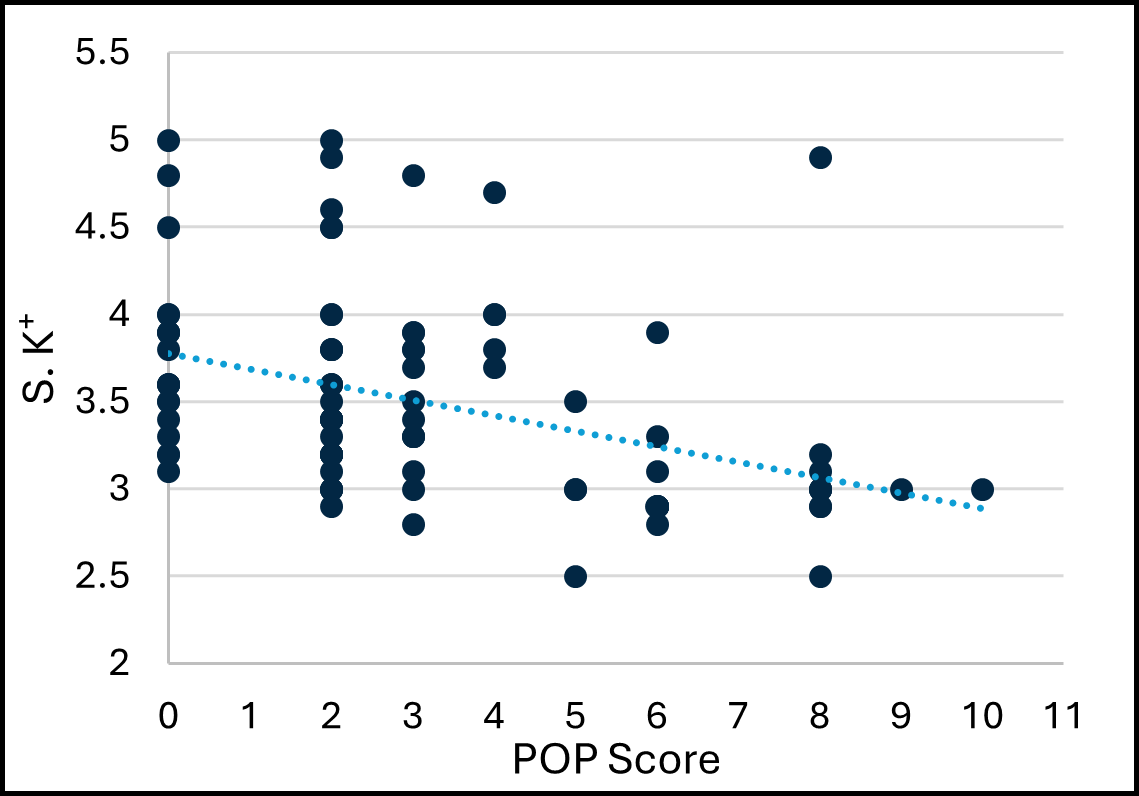
Monocrotophos was the most consumed OP compound (28%) (Figure-1). Vomiting was the most frequently reported symptom (78%), and most patients reached the hospital within eight hours of poisoning. On admission, patients were assessed using the Peradeniya Organophosphorus Poisoning (POP) score, with the majority (68%) classified as having mild poisoning. Of the 100 patients, 76 showed improvement during treatment. However, 34 patients required ventilator support, and among them, 24 succumbed to complications. Additionally, 56% of patients presented with hypokalaemia. There is statistically significant association was observed between hypokalaemia and outcome of OP Poisoning (Table-3). Correlation with other clinical parameters is given in Table-4 and Figure-2.
Discussion
Organophosphate (OPC) compounds are widely used in agriculture, particularly in developing countries like India, where their easy accessibility and lack of strict regulations have contributed to rising cases of accidental and suicidal poisoning.[11,12] The primary toxic mechanism involves acetylcholinesterase inhibition, leading to excessive stimulation of muscarinic and nicotinic receptors, resulting in a rapid cholinergic crisis that forms the basis for diagnosis. Respiratory failure is the leading cause of morbidity and mortality, often necessitating ventilator support and ICU care. Hypokalaemia is a common finding in OPC poisoning, exacerbating muscle weakness and potentially worsening the severity of poisoning. A cross-sectional observational study was conducted at a tertiary care hospital on 100 OPC poisoning cases to examine the correlation between serum potassium levels, poisoning severity, and patient outcomes.
Maximum number of patients were between age group of 19-45 years (56%), followed by 46-65 years (29%). Similar studies done by Goel et al.[13] and Rehman et al.[14] have shown that OPC poisoning is common in the age group of 21-30 years. The predominance in young adults reflects the emotional conflicts that are prevalent in this age group. Majority of the patients in the study group were males (77%). Similar male preponderance was observed by Goel et al.[13] and Rajeev H et al.[15] also in their studies.
The most common compound consumed by patients in present study was Monocrotophos (28%) followed by Chlorpyrifos and Profenofos. Study done by Subedi B et al.[16] showed that most common compound used was Malathion and Rajeev H et al.[15] showed that it was Methyl Parathion. The availability of specific compounds may differ across regions, reflecting variations in local agriculture and economic status. Present study reveals that 97% of patients consumed poison with an intention of suicide and 3% were accidental exposures. These values correlate with observations made by Kozaci et al.[17] (85%) and Goet et al.[13] (96.1%). OPC compounds are easily accessible pesticides in agriculture and cheaper, and it may be the reason why it is used as a common mode of attempting suicide. Another reason could be nearly half of the patients included in the study were occupied in the agriculture work.
The commonest symptom encountered was vomiting (78%), followed by dizziness (50%). Convulsion was relatively uncommon presentation and was reported only in 10% of the patients. These observations are similar to the study findings by Rajeev H et al.[15] and Subedi Bet et al.[16]
Majority of patients (68%) had mild grade of poisoning according to POP scale. Nearly 20% had moderate grade poisoning and only 12% had severe grade poisoning. These observations were comparable to the studies done by Malaviya N et al.[18] In present study, nearly 56% patients had hypokalaemia at the time of presentation and rest 44% patients had normal serum potassium levels. A study by Murthy DR et al.[19] has also shown that hypokalaemia is a frequent finding in OP poisoning.
Majority of patients (75%) who fall into moderate and severe categories of POP score have hypokalaemia as compared to patients who fall into mild category. This difference was statistically significant (p= .011). These observations were comparable to the studies done by Namba T et al.[20] and Basnet D et al.[21]
In present study, Mean serum K⁺ level and mean S. AchE level was significantly lower in patients who needed ventilator support than patients who didn’t needed ventilator support. Hypokalaemia may aggravate OP induced respiratory muscle weakness. Patients who had hypokalaemia at the time of presentation likely to need ventilator support during course of treatment. Mean serum potassium in ventilator requiring patients was 3.07 and in others was 3.71. These observations were found to be statistically significant. (p=<.001) These findings are supported by the findings of Murthy et al.[19] has proposed serum potassium at the time of admission as a predictive marker of ventilator support. Bijush D et al.[22] also observed that patients with organophosphorus poisoning with low serum potassium level had developed more complications with increased need for ICU admission, higher need for ventilator support.
Mean serum K⁺ level and mean S. AchE level was significantly lower in patients who died than patients who survived. This difference between serum K⁺ and S. AchE level in deaths and discharges was statistically significant. (p=.001, p= .008). Mean serum potassium in patients who expired was 3.04 and in patients who survived was 3.64. These observations were found to be statistically significant (p=<.001). These observations were comparable to the studies done by Bijush D et al.[22], Prasad M et al.[23]. In Lyzhnikov EA et al.[24] study death occurred in 29 patients who are found to have hypokalaemia. Tripathy SK et al.[25] also observed that hypokalaemia is associated with high morbidity and mortality in OPC Poisoning. Hypokalaemia in patients with OP poisoning may cause arrhythmia and cardiac arrest leading to death.
Conclusion
This study, conducted on 100 patients with organophosphate (OP) poisoning, highlights the significant correlation between serum potassium levels, poisoning severity, and patient outcomes. The majority of cases involved young adults (19–45 years), predominantly male agricultural labourers, with Monocrotophos being the most commonly consumed compound. Vomiting was the most frequently reported symptom, and most patients presented within eight hours of poisoning.
Assessment using the Peradeniya Organophosphorus Poisoning (POP) score revealed that 68% had mild poisoning, while 56% had hypokalaemia at admission. The need for ventilator support and mortality rates were significantly higher in patients with severe poisoning and lower serum potassium levels. Hypokalaemia was more prevalent in patients with higher poisoning severity. The study establishes a statistically significant association between low serum potassium and acetylcholinesterase levels with increased severity, ventilator dependency, and mortality in OP poisoning cases.
Declaration
Conflict of Interest: None
Funding: Nill
AI: No artificial intelligence tool has been used for writing or editing purpose in this manuscript.
References
- Chitra GA, Muraleedharan VR, Swaminathan T, Veeraraghavan D. Use of Pesticides and Its Impact on Health of Farmers in South India. Int J Occup Environ Health 2006;12(3):228–33. doi:10.1179/oeh.2006.12.3.228
- Peter J V., Cherian AM. Organic Insecticides. Anaesth Intensive Care 2000;28(1):11–21. doi:10.1177/0310057X0002800102
- Sumathi M, Kumar Sh, Shashidhar K, Takkalaki N. Prognostic significance of various biochemical parameters in acute organophosphorus poisoning. Toxicol Int 2014;21(2):167. doi:10.4103/0971-6580.139800
- Pore NE, Pujari KN, Jadkar SP. Organophosphorus Poisoning. Int J Pharma Bio Sci 2011;2(4):604-612
- Medical Toxicology . 3rd ed. Philadelphia: Lippincott, Williams & Wilkins; 2004.
- Bhattacharyya K, Sarkar R, Phaujdar S, Mullick O. Serum creatine phosphokinase: A probable marker of severity in organophosphorus poisoning. Toxicol Int 2011;18(2):117. doi:10.4103/0971-6580.84263
- Kamanyire R, Karalliedde L. Organophosphate toxicity and occupational exposure. Occup Med (Lond) 2004;54(2):69–75. doi:10.1093/OCCMED/KQH018
- Balali-Mood M, Balali-Mood K. Neurotoxic disorders of organophosphorus compounds and their managements. Arch Iran Med 2008;11(1):65–89
- Eddleston M, Mohamed F, Davies JOJ, Eyer P, Worek F, Sheriff MHR, et al. Respiratory failure in acute organophosphorus pesticide self-poisoning. QJM 2006;99(8):513–22. doi:10.1093/QJMED/HCL065
- Senanayake N, de Silva HJ, Karalliedde L. A scale to assess severity in organophosphorus intoxication: POP scale. Hum Exp Toxicol 1993;12(4):297–9. doi:10.1177/096032719301200407
- Akyildiz BN, Kondolot M, Kurtoǧlu S, Akin L. Organophosphate intoxication presenting as diabetic keto-acidosis. Ann Trop Paediatr 2009;29(2):155–8. doi:10.1179/146532809X440789
- Karalliedde LD, Edwards P, Marrs TC. Variables influencing the toxic response to organophosphates in humans. Food and Chemical Toxicology 2003;41(1):1–13. doi:10.1016/S0278-6915(02)00232-6
- Goel A, Joseph S, Dutta TK. Organophosphate poisoning: predicting the need for ventilatory support. J Assoc Physicians India 1998;46(9):786–90
- Rehiman S, Lohani SP, Bhattarai MC. Correlation of serum cholinesterase level, clinical score at presentation and severity of organophosphorous poisoning. JNMA J Nepal Med Assoc 2008;47(170):47–52
- Rajeev H, Arvind MN. Study Of Clinical And Biochemical Parameters In Predicting The Need For Ventilator Support In Organophosphorus Compound Poisoning J of Evolution of Medical and Dental Sciences 2013;2(49):9555-9570
- Subedi B, Yadav GK, Raut A, Joshi N, Subedi BK, Joshi N, et al. The relationship of serum amylase levels in acute organophosphorus poisoning with its clinical severity and outcome: a cross-sectional study. Annals of Medicine and Surgery 2023;85(4):778. doi:10.1097/MS9.0000000000000433
- Kozaci N, Gokel Y, Acikalin A, Satar S. Factors Affecting the Prognosis in Acute Insecticide Intoxications Containing Organic Phosphorus. Journal of Academic Emergency Medicine 2012;11(2):93–7. doi:10.5152/jaem.2012.023
- Malaviya NB, Parikh R, Pancholi K, Belim OB. Assessment of the Peradeniya Organophosphorus Poisoning Scale as a Severity and Prognostic Marker in Patients With Acute Organophosphorus Poisoning Presenting to an Emergency Medicine Department. Cureus 2023;15(6). doi:10.7759/CUREUS.40277
- Prasad DRMM. Reduced Levels of Serum Potassium and Plasma Cholinesterase in Acute Asia Pacific Journal of Medical Toxicology 2024;3(2):68-72.
- Namba T, Nolte CT, Jackrel J, Grob D. Poisoning due to organophosphate insecticides. Am J Med 1971;50(4):475–92. doi:10.1016/0002-9343(71)90337-8.
- Basnet D, Shakya YL, Gupta S, Shah NA, Gupta B, Yadav M. Serum Potassium Level in Acute Organophosphorus Poisoning and its Correlation with Severity in Patients Presenting to Emergency Room in a Tertiary Hospital. Journal of Karnali Academy of Health Sciences 2024;7(2). doi:10.61814/JKAHS.V7I2.943
- Difoesa B, Jyoti Sharma D, Deb D. Significance of Serum Potassium Level at Admission in Organophosphorus Poisoning and Impact on Outcome-A Hospital Based Study from North East India. Original Research Article J Evid Based Med Healthc 2021;8:2349–562. doi:10.18410/jebmh/2021/596
- Mahadeshwara Prasad DR, Gouda H. A Study of Acute Organophosphate Poisoning at a Tertiary Hospital, Belgaum, Karnataka. Medico-Legal Update 2012;12:75–9
- Lyzhnikov EA, Savina AS, Shepelev VM. [Pathogenesis of disorders of cardiac rhythm and conductivity in acute organophasphate insecticide poisoning]. Kardiologiia 1975;15(9):126–9.
- Tripathy SK, Rout PK, Debta N, Das S, Panigrahi M, Mishra SK, et al. Study of clinical profile of organophosphorus poisoning with special reference to electrocardiographic changes and electrolyte derangement. International Journal of Advances in Medicine 2018;5(1):50–6. doi:10.18203/2349-3933.IJAM20175520
